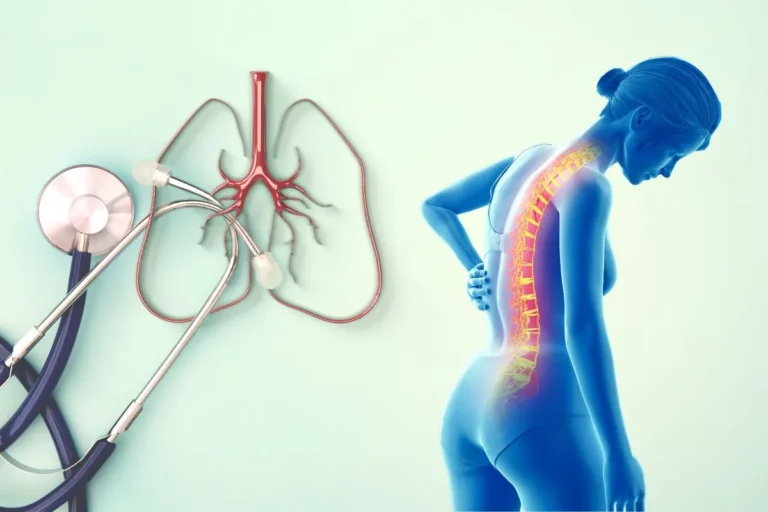
Ankylosing Spondylitis and Lung Disease
Have you ever wondered if your back pain could be connected to your breathing difficulties? 🤔 For those living with Ankylosing Spondylitis (AS), this seemingly unlikely connection might be more than just a coincidence. AS, a chronic inflammatory condition primarily affecting the spine, has long been associated with joint pain and stiffness. However, recent research has unveiled a surprising link between this spine condition and lung health.
Imagine waking up one day to find that the same condition causing your back pain might also be silently affecting your lungs. 😮 This hidden connection between AS and lung disease is not only unexpected but potentially life-altering for those affected. As we delve deeper into this intriguing relationship, we’ll explore how AS can impact your respiratory system, the risks involved, and most importantly, what you can do about it.
Join us as we unravel the mystery behind the hidden link between Ankylosing Spondylitis and lung disease. We’ll guide you through understanding AS, exploring the lung-spine connection, unveiling hidden risks, recognizing warning signs, and discovering effective management strategies. By the end of this journey, you’ll be equipped with the knowledge to better manage your health and breathe a little easier. 💪🫁

Understanding Ankylosing Spondylitis
A. Definition and symptoms
Ankylosing spondylitis (AS) is a chronic inflammatory condition primarily affecting the spine and sacroiliac joints. This autoimmune disorder causes inflammation, pain, and stiffness, potentially leading to fusion of the vertebrae over time. Common symptoms include:
- Lower back pain and stiffness
- Fatigue
- Reduced spine flexibility
- Pain in other joints (hips, shoulders, knees)
- Eye inflammation (uveitis)
B. Impact on quality of life
AS significantly affects patients’ daily activities and overall well-being:
| Aspect | Impact |
|---|---|
| Physical | Limited mobility, chronic pain |
| Emotional | Anxiety, depression, stress |
| Social | Reduced social interactions |
| Occupational | Decreased work productivity |
C. Diagnosis and treatment options
Diagnosing AS involves a combination of clinical examination, imaging tests, and blood work. Treatment aims to manage symptoms and slow disease progression:
- Medications:
- NSAIDs for pain relief
- DMARDs to slow disease progression
- Biologics for severe cases
- Physical therapy and exercise
- Lifestyle modifications
- Surgery (in advanced cases)
D. Causes and risk factors
While the exact cause of AS remains unknown, several factors contribute to its development:
- Genetic predisposition (HLA-B27 gene)
- Environmental triggers
- Age (onset typically in young adulthood)
- Gender (more common in males)
Understanding these aspects of AS is crucial for recognizing its potential impact on various body systems, including the lungs. Next, we’ll explore the intricate connection between AS and lung disease, shedding light on how this spinal condition can affect respiratory health.

Exploring the Lung-Spine Connection
Now that we understand the basics of Ankylosing Spondylitis (AS), let’s delve into its surprising connection with lung disease. This relationship is often overlooked but can significantly impact patient health and treatment strategies.
The importance of early detection
Early detection of lung involvement in AS patients is crucial for better outcomes. Regular lung function tests and chest imaging can help identify potential issues before they become severe. Here’s a comparison of early vs. late detection:
| Early Detection | Late Detection |
|---|---|
| Better prognosis | More severe symptoms |
| Easier management | Complicated treatment |
| Preserved lung function | Reduced lung capacity |
| Improved quality of life | Increased morbidity |
Shared genetic factors
Research has uncovered shared genetic factors between AS and certain lung diseases, particularly:
- HLA-B27 gene: Associated with both AS and increased risk of lung issues
- IL-23R gene: Linked to inflammatory pathways in both conditions
- CARD15 gene: Implicated in immune responses affecting joints and lungs
Inflammation’s role in both conditions
Chronic inflammation plays a central role in both AS and lung diseases. This inflammatory cascade can:
- Cause tissue damage in the spine and lungs
- Lead to fibrosis in both areas
- Trigger systemic effects throughout the body
- Exacerbate symptoms in both conditions
Common respiratory issues in AS patients
AS patients often experience various respiratory problems, including:
- Chest wall rigidity
- Reduced lung capacity
- Interstitial lung disease
- Upper lobe fibrosis
- Sleep apnea
Understanding these connections is vital for comprehensive AS management. Next, we’ll explore the hidden risks associated with this lung-spine relationship.

Unveiling the Hidden Risks
Now that we understand the connection between ankylosing spondylitis (AS) and lung health, let’s explore the hidden risks associated with this relationship.
A. Potential for interstitial lung disease
Interstitial lung disease (ILD) is a significant concern for individuals with AS. This condition causes inflammation and scarring of the lung tissue, leading to breathing difficulties and reduced oxygen absorption. Studies have shown that up to 65% of AS patients may develop some form of ILD during their lifetime.
B. Sleep apnea and breathing difficulties
AS can contribute to sleep apnea and other breathing difficulties, particularly due to chest wall rigidity. The inflammation and stiffness in the spine and ribcage can restrict lung expansion, making it challenging to breathe deeply, especially during sleep.
| Sleep Apnea Symptoms | Impact on AS Patients |
|---|---|
| Loud snoring | More common due to restricted airways |
| Gasping for air | Increased risk due to chest wall rigidity |
| Daytime fatigue | Exacerbated by AS-related pain and stiffness |
C. Reduced lung capacity and function
As AS progresses, it can lead to a decrease in lung capacity and overall pulmonary function. This reduction is often due to:
- Chest wall stiffness
- Limited rib cage mobility
- Weakened respiratory muscles
These factors combined can result in restrictive lung disease, making it harder for patients to breathe normally and engage in physical activities.
D. Increased susceptibility to lung infections
Individuals with AS may be more prone to lung infections due to:
- Compromised lung function
- Weakened immune system (often from AS treatments)
- Reduced ability to clear secretions effectively
This increased susceptibility highlights the importance of regular check-ups and preventive measures for AS patients.
With these hidden risks in mind, it’s crucial for individuals with AS to be aware of potential lung complications and work closely with their healthcare providers to monitor and manage their respiratory health. Next, we’ll explore the warning signs that may indicate developing lung issues in AS patients.
Recognizing Warning Signs
As ankylosing spondylitis (AS) progresses, it can affect the lungs and respiratory system. Being aware of the warning signs is crucial for early detection and management of potential lung complications. Here are the key indicators to watch out for:
A. Changes in posture affecting breathing
AS often causes spine stiffness and fusion, leading to postural changes that can impact breathing:
- Reduced chest expansion
- Forward curvature of the upper spine (kyphosis)
- Difficulty taking deep breaths
B. Fatigue and reduced exercise tolerance
Patients with AS-related lung issues may experience:
- Increased tiredness during daily activities
- Decreased ability to perform physical tasks
- Longer recovery times after exercise
C. Persistent cough or chest pain
Lung involvement in AS can manifest as:
- Dry, persistent cough
- Chest discomfort or pain, especially during deep breathing
- Feeling of tightness in the chest
D. Shortness of breath during physical activity
Breathing difficulties are a common sign of lung complications in AS:
- Dyspnea (shortness of breath) during mild to moderate exertion
- Rapid breathing or feeling of air hunger
- Need for frequent breaks during activities
| Warning Sign | Description | Action |
|---|---|---|
| Postural changes | Reduced chest expansion, kyphosis | Consult rheumatologist |
| Fatigue | Increased tiredness, reduced exercise tolerance | Discuss with healthcare provider |
| Cough/Chest pain | Persistent dry cough, chest discomfort | Seek medical evaluation |
| Shortness of breath | Dyspnea during physical activity | Urgent medical assessment |
Recognizing these warning signs early can lead to prompt intervention and better management of AS-related lung complications. If you experience any of these symptoms, it’s essential to discuss them with your healthcare provider. Next, we’ll explore effective strategies for managing both AS and its potential lung-related issues.

Effective Management Strategies
Now that we’ve explored the hidden risks and warning signs, let’s dive into effective management strategies for individuals dealing with both ankylosing spondylitis (AS) and lung disease.
A. Importance of a multidisciplinary approach
Managing the complex interplay between AS and lung disease requires a team of specialists working together. This approach ensures comprehensive care and better outcomes for patients.
| Specialist | Role |
|---|---|
| Rheumatologist | Manages AS symptoms and progression |
| Pulmonologist | Addresses lung-related issues |
| Physiotherapist | Designs exercise programs for mobility and breathing |
| Nutritionist | Provides dietary guidance to support overall health |
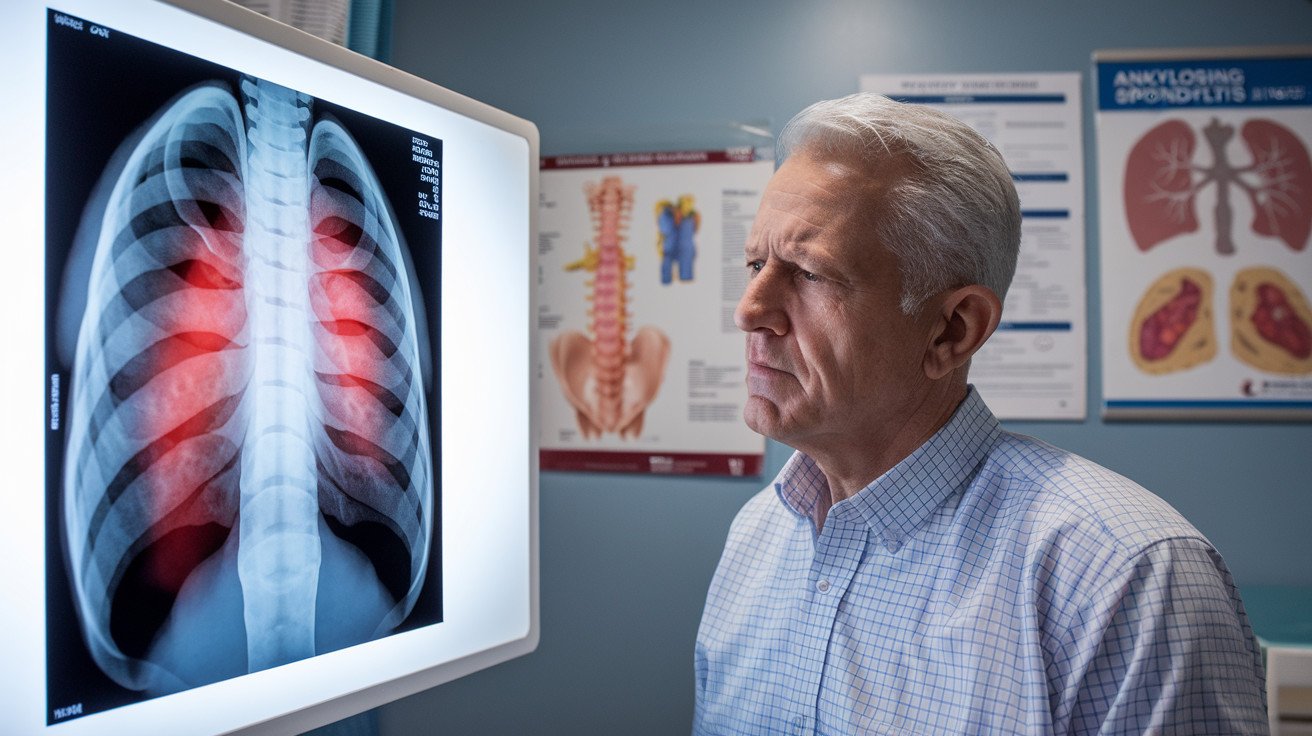
B. Regular monitoring and follow-ups
Consistent check-ups are crucial for early detection and management of lung complications in AS patients. This includes:
- Regular lung function tests
- Chest X-rays or CT scans
- Blood tests to monitor inflammation levels
C. Lifestyle modifications for better lung health
Implementing healthy habits can significantly improve both AS and lung health:
- Quit smoking
- Maintain a healthy weight
- Stay physically active
- Practice good posture
- Avoid exposure to environmental pollutants
D. Breathing exercises and pulmonary rehabilitation
Targeted exercises can improve lung capacity and chest wall flexibility:
- Diaphragmatic breathing
- Pursed-lip breathing
- Chest expansion exercises
Pulmonary rehabilitation programs offer structured support and education for managing respiratory symptoms effectively.
E. Medications targeting both AS and lung issues
Treatment plans often involve medications that address both conditions:
- NSAIDs for pain and inflammation
- Biologic drugs like TNF inhibitors
- Bronchodilators for improved lung function
- Corticosteroids for acute flare-ups
By implementing these management strategies, individuals with AS can better control their symptoms and reduce the risk of lung complications. Next, we’ll explore the importance of patient education and support in living with AS and lung disease.

Ankylosing spondylitis, while primarily affecting the spine, has far-reaching implications for overall health, particularly lung function. The intricate connection between this inflammatory condition and respiratory health underscores the importance of comprehensive care and vigilant monitoring. By recognizing the potential risks and warning signs, individuals with ankylosing spondylitis can take proactive steps to protect their lung health.
Empowering yourself with knowledge and partnering with healthcare professionals are crucial steps in managing ankylosing spondylitis and mitigating its impact on lung health. Regular check-ups, maintaining a healthy lifestyle, and adhering to prescribed treatments can significantly improve quality of life and reduce the risk of complications. Remember, early detection and intervention are key to preserving both spinal and respiratory health in the face of this challenging condition.
Read more about 10 Life-Changing Ankylosing Spondylitis Self-Care Hacks You Never Knew Existed
Read more about AS